What is the Secret to managing Urinary Incontinence In Menopause?
Managing urinary incontinence during menopause involves a multifaceted approach that addresses both the physical changes of the body and lifestyle modifications. Here are some of the most effective strategies:
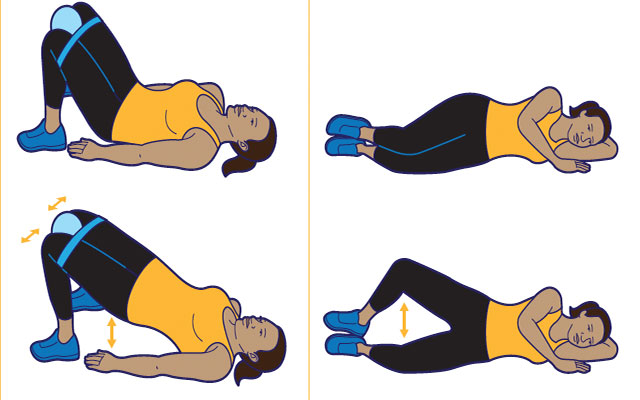
1. Pelvic Floor Exercises (Kegels)
-
Strengthening the Pelvic Floor: Pelvic floor muscles weaken during menopause due to reduced estrogen levels, which can lead to stress urinary incontinence (leaking when coughing, sneezing, or laughing). Regular Kegel exercises can help restore muscle strength and improve bladder control.
-
Practice: Contract your pelvic floor muscles for 5-10 seconds, then relax. Do 3-4 sets of 10-15 repetitions daily. Over time, this helps improve the muscles’ ability to support the bladder and urethra.
2. Hormone Replacement Therapy (HRT)
-
Estrogen Decline: Menopause causes a significant drop in estrogen levels, which weakens the tissues of the bladder and urethra. This makes it harder to control urine flow and increases the risk of incontinence.
-
HRT: Topical estrogen (in the form of creams, rings, or vaginal tablets) can help rejuvenate the tissues in the urinary tract, potentially reducing incontinence. Consult a healthcare provider to assess whether HRT is appropriate for your situation.
3. Bladder Training
-
Rebuilding Bladder Control: Bladder training involves teaching your bladder to hold more urine by increasing the time between trips to the bathroom. It helps reset your bladder’s signals to urinate.
-
Practice: Start by noting how often you urinate and gradually extend the time between bathroom visits by 15-30 minutes every few days. The goal is to stretch the bladder’s capacity to hold urine for longer periods.
4. Dietary Adjustments
-
Avoid Bladder Irritants: Certain foods and beverages can irritate the bladder, increasing the urge to urinate or worsening leakage. Avoid or limit:
-
Caffeine (coffee, tea, soda)
-
Alcohol
-
Spicy foods
-
Citrus fruits and juices
-
Artificial sweeteners
-
-
Hydration: While reducing bladder irritants is important, don’t cut back on water excessively, as this can lead to concentrated urine, which also irritates the bladder.
5. Weight Management
-
Obesity and Incontinence: Extra weight places added pressure on the pelvic floor and bladder, exacerbating incontinence symptoms. Even modest weight loss can significantly reduce leakage episodes.
-
Exercise: Regular physical activity, particularly low-impact exercises like walking, swimming, or yoga, can help maintain a healthy weight and improve bladder control.
6. Manage Constipation
-
Link Between Constipation and Incontinence: Straining during bowel movements puts pressure on the pelvic floor, which can weaken the muscles over time and worsen urinary incontinence.
-
Solution: Increase dietary fiber (whole grains, fruits, vegetables) and stay hydrated to prevent constipation. Regular bowel movements help reduce the strain on the pelvic floor.
7. Proper Bladder Emptying
-
Double Voiding: Ensure you are completely emptying your bladder when you go to the bathroom. After you urinate, wait a few seconds and try to urinate again (double voiding). This can help minimize the feeling of urgency or leakage soon after voiding.
8. Diaphragmatic Breathing and Posture
-
Core and Pelvic Floor Connection: Proper breathing techniques, especially diaphragmatic breathing, help manage intra-abdominal pressure, which can influence bladder control. When you breathe deeply, your diaphragm and pelvic floor muscles work together, creating balanced pressure in the core.
-
Good Posture: Maintaining a neutral spine and avoiding slouching helps reduce unnecessary pressure on the bladder and pelvic floor muscles.
9. Medications
-
Pharmaceutical Options: In some cases, medications may be prescribed to manage overactive bladder symptoms, such as anticholinergics (oxybutynin, tolterodine) or beta-3 agonists (mirabegron), which can help relax the bladder and reduce urgency.
10. Vaginal Devices or Surgery (In Advanced Cases)
-
Pessaries: A vaginal pessary is a device inserted into the vagina to support the bladder and prevent incontinence, particularly in cases of pelvic organ prolapse.
-
Surgical Options: For severe cases, surgery like sling procedures may be considered to provide long-term relief from incontinence. Surgery is typically a last resort after other treatments have been tried.
11. Mindful Bathroom Habits
-
Scheduled Voiding: Instead of waiting until you have a strong urge to urinate, schedule bathroom visits at regular intervals, such as every 2-3 hours. This can prevent urgency and reduce leakage incidents.
-
Proper Hydration Timing: Be mindful of when you drink fluids—try to avoid large amounts of fluid close to bedtime to reduce nighttime trips to the bathroom.
12. Pelvic Floor Therapy
-
Physical Therapy: A specialized pelvic floor physical therapist can guide you through targeted exercises to strengthen and rehabilitate the pelvic muscles. Therapy may include biofeedback to monitor pelvic floor activity and teach you how to properly engage and relax the muscles.
13. Lifestyle Changes
-
Quit Smoking: Smoking can contribute to chronic coughing, which puts pressure on the pelvic floor and increases the risk of incontinence.
-
Alcohol Reduction: Alcohol acts as a bladder irritant, so reducing alcohol intake may decrease leakage incidents.
Main Ideas:
The secret to managing urinary incontinence during menopause lies in a combination of pelvic floor exercises, hormone balance (such as topical estrogen), bladder training, and lifestyle adjustments. Addressing factors like weight, diet, and stress on the pelvic floor can also contribute to better bladder control. Each woman’s situation is unique, so finding the right combination of treatments is key to managing symptoms effectively.