The most impactful strategies for managing urinary incontinence during menopause
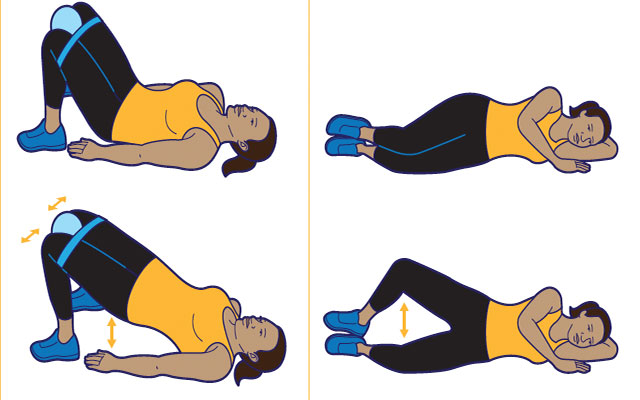
1. Pelvic Floor Exercises (Kegels)
How to Perform Kegels Correctly?
- Step 1: Identify the right muscles by trying to stop the flow of urine midstream (but don’t do this often as it can disrupt normal bladder function). The muscles you use to do this are your pelvic floor muscles.
- Step 2: Contract these muscles for 5 seconds, hold, then relax for 5 seconds. As you get stronger, aim to hold for 10 seconds.
- Step 3: Perform 3-4 sets of 10-15 repetitions each day.
- Tip: Make sure you’re not tightening your stomach, thighs, or buttocks while doing Kegels. Focus on isolating the pelvic floor.
Benefits: Over time, regular Kegel exercises improve muscle strength and control, reducing both stress incontinence (leaking when sneezing, coughing) and urge incontinence (a sudden need to urinate).
2. Hormone Replacement Therapy (HRT)
How Topical Estrogen Helps?
- Why It Works: Estrogen helps maintain the elasticity, strength, and moisture of the vaginal and urethral tissues. During menopause, estrogen levels decline, leading to thinning of these tissues, which can cause or worsen urinary incontinence.
- Options:
- Vaginal Creams: Applied locally to the vaginal area to improve tissue health. Examples include Estrace and Premarin.
- Vaginal Rings: Devices like Estring that release a steady dose of estrogen.
- Vaginal Tablets: Small tablets inserted into the vagina (such as Vagifem).
Consultation: Always discuss with a healthcare provider to see if HRT is suitable for you, considering potential risks and benefits.
3. Bladder Training
Steps for Bladder Training:
- Step 1: Keep a bladder diary for a few days, recording the times you urinate and when you experience leakage.
- Step 2: Begin by scheduling bathroom visits every 1-2 hours, whether or not you feel the urge to go.
- Step 3: Gradually increase the time between visits by 15-30 minutes every few days. The goal is to increase the bladder's ability to hold urine.
- Step 4: Practice "double voiding" (after you urinate, wait a few seconds and try again) to ensure the bladder is fully emptied.
Benefits: Bladder training helps reduce frequent urges, increases bladder capacity, and retrains your bladder to follow a more controlled schedule.
4. Diaphragmatic Breathing and Core Connection
How Diaphragmatic Breathing Helps:
- Step 1: Sit or lie down in a comfortable position. Place one hand on your chest and the other on your abdomen.
- Step 2: Breathe deeply in through your nose, allowing your abdomen to rise while your chest stays relatively still. This engages the diaphragm and core.
- Step 3: Exhale slowly through your mouth, engaging your pelvic floor muscles (similar to a Kegel) as you breathe out.
- Step 4: Practice this for 5-10 minutes daily.
Benefits: Proper breathing helps regulate intra-abdominal pressure, which reduces the strain on the pelvic floor. This can prevent further weakening and improve bladder control.
5. Lifestyle Adjustments (Diet, Weight, and Hydration)
Dietary Tips to Prevent Bladder Irritation:
- Avoid Irritants: As mentioned earlier, limit or avoid caffeine, alcohol, spicy foods, and acidic foods like citrus, as these can aggravate the bladder.
- Hydration: Drink enough water to stay hydrated but avoid overloading your bladder by spacing out your fluid intake throughout the day.
Weight Management:
- Carrying extra weight puts additional pressure on your bladder and pelvic floor, so maintaining a healthy weight can reduce symptoms of incontinence.
- Regular exercise, particularly walking, swimming, and low-impact workouts, helps manage weight and strengthens core muscles that support bladder function.
6. Medications for Urinary Incontinence
Types of Medications:
- Anticholinergics: Help reduce overactive bladder symptoms by calming the bladder muscles (e.g., oxybutynin, tolterodine).
- Beta-3 Agonists: Relax the bladder muscle to increase its storage capacity (e.g., mirabegron).
- Topical Estrogen: Can help rejuvenate the bladder and urethral tissues, improving symptoms in some women.
When to Use Medications: If lifestyle changes, pelvic floor exercises, and bladder training don’t provide enough relief, medications can help control overactive bladder or improve stress incontinence. Consult your doctor for personalized advice.
7. Pelvic Floor Physical Therapy
- Why It Helps: A pelvic floor physical therapist can guide you through personalized exercises to strengthen the pelvic muscles, reduce tension, and improve coordination.
- Biofeedback: This technique uses sensors to monitor pelvic floor muscle activity, allowing you to see which muscles are being activated. This feedback helps you improve your technique and ensure you’re engaging the right muscles.
- Manual Therapy: Some therapists may use internal and external techniques to help release tight muscles, realign the pelvic floor, and improve muscle function.
8. Pessaries and Surgical Options
- Pessaries: A pessary is a device inserted into the vagina to support the bladder and prevent leakage, especially in cases of pelvic organ prolapse.
- Surgery: In severe cases of urinary incontinence, especially when pelvic floor exercises and other treatments aren’t effective, surgery may be considered. Sling procedures, for example, help lift and support the bladder.